Ibogaine Treatment for Suboxone and Buprenorphine Addiction
Subutex and suboxone are opioids, and their long-term use poses health risks. Therapeutic doses of opioids can affect your life at work, school, and home — but this is just the tip of the iceberg. In addition to these side effects, there are many acute side effects of suboxone that happen immediately after a single dose. These side effects include:
- Chills
- Cold and clammy skin
- Cold sweat
- Confusion
- Dizziness
- Lightheadedness
- Fainting
- Fever
- Shallow breathing and/or shortness of breath
- Chest tightness
- Slow pulse
- Seizures
- Twitching
Three opioid use side effects are of particular note:
- Gastroparesis: Also referred to as delayed gastric emptying, gastroparesis slows or stalls how fast food moves from the stomach to the small intestine. It causes tenderness, bloating, pain, heartburn, excess gas, increased appetite, and weight loss.
- Hyperalgesia: Commonly referred to as hypersensitivity to pain, hyperalgesia causes the nervous system to become too sensitive to various stimuli. It may also cause muscle rigidity and trigger the prolonged contraction of muscles that causes pain, cramps, and twitching.
- Myoclonus: Myoclonus to the involuntary, sudden twitching or jerking of one or more muscles. It causes uncontrollable motor movements.
Try Ibogaine Treatment for Suboxone Addiction Now
Mood Swings and Opioids: What You Need to Know
Opioids produce a high that affects the brain’s chemical balance, and they change how the brain experiences rewards and pleasure. Much in the same way that opioids have far-flung effects on your mind and body, suboxone does the same.
Opioids and suboxone both relieve pain, sedate the mind, and produce feelings of euphoria and drowsiness. They help slow all parts of your cognitive process — including your reaction time. Therefore, if you use opioids or suboxone, you likely won’t be able to respond quickly as a driver, or judge a situation well at work, school, or home. Long-term suboxone users may also experience paranoia — despite their feelings of intense high. For people dealing with mental illness, opioids can make existing problems far worse than ever before.
How Long Does Suboxone Block Opiates?
Suboxone is one of several medications used to reduce symptoms of drug withdrawal and promote recovery from prolonged use and abuse of illicit opiates. It mimics some of the effects that opiates trigger in the brain. Suboxone also helps reduce the body’s need for the original opiate drug of choice. On the other hand, this mimicry comes at a price.
In general, suboxone guards against cravings for opiates for approximately 24 hours, which is one of the reasons why most doctors who treat with suboxone instruct their patients to take the medication at the same time every day. Many things can alter how long suboxone blocks opiates or the impact of coming off suboxone, such as:
- Your height and weight
- history of drug abuse
- Metabolism
All of these factors can either shorten or extend the amount of time suboxone blocks an opiate’s effects. Compared to illicit opiates, suboxone is long-lasting and safe; it can block an opiate for up to three days after your last dose. However, it is important to remember that suboxone is still an opiate, and it is unpredictable. Ideally, you should work with your doctor to customize your suboxone dose based on your addiction and medical history.
How Does Suboxone Work?
Suboxone consists of a combination of naloxone and buprenorphine, medications that help prevent withdrawal symptoms during opiate addiction recovery. Naloxone is an opiate antagonist, while buprenorphine acts as a partial agonist-antagonist. The two drugs together act much like opiates in the brain. Yet the risks from suboxone are reduced, compared to traditional opiates.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), buprenorphine can produce euphoric effects in users, but those effects are weaker than any euphoria created by standard opiates. Furthermore, taking large doses of buprenorphine fails increase the drug’s euphoric effects over time. This limits the chances that patients will abuse suboxone. But in some instances, people still become dependent on it while they try to treat an opiate addiction.
Coming Off Suboxone
According to SAMHSA, there are three phases used as part of suboxone treatment:
- Induction
- Stabilization
- Maintenance
Suboxone treatment starts with the induction phase, which begins 12 to 24 hours after the last dose of an opiate. Treatment should start before opiate symptoms worsen during withdrawal.
After withdrawal symptoms and cravings subside, the stabilization phase of suboxone treatment begins. At this point, the patient experiences few, if any, symptoms of opioid use. The supervising physician may adjust the patient’s dose of suboxone and frequency based on his or her individual needs.
Finally, the patient reaches the maintenance phase of treatment. This phase involves a steady, long-term dose of suboxone that is eventually tapered off under medical supervision.
How to Get Off Suboxone
Getting off suboxone may be challenging, and an individual may experience various side effects. According to the US National Library of Medicine, common side effects of suboxone include:
- Blurry vision
- Constipation
- Disturbed sleep, trouble sleeping
- Headache
- Mouth or tongue pain and/or numbness
- Stomach pain
- Nausea
- Vomiting
To avoid these side effects, a doctor may sometimes recommend a suboxone alternative like buprenorphine.
A Closer Look at Ibogaine for Buprenorphine Addiction
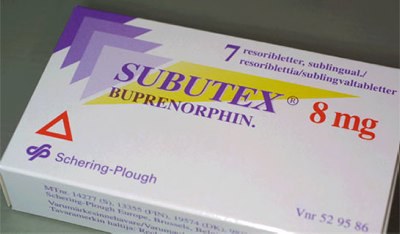
The buprenorphine molecule was introduced by British company Reckitt Benckiser (known as Reckitt & Colman at the time) in 1978. It was offered as an injection to treat severe pain and released as a sublingual formulation in 1982.
Buprenorphine is a narcotic analgesic. It acts as a partial agonist/antagonist that works against opiate receptors, even at low doses (2 mg). In addition to buprenorphine’s receptor blocking, when naloxone is mixed into the drug (suboxone), buprenorphine delivers an additional μ-opioid receptor blocker.
In October 2002, the US FDA approved buprenorphine (using the brand names Subutex and Suboxone) for use in opioid maintenance. The Drug Addiction Treatment Act of 2000 made it possible for physicians who received special training in their use, to prescribe Schedule III, IV, and V narcotic analgesics like Buprenex for the purpose of treating addiction with substitution therapy. To put it simply: within the United States a clinician can prescribe Subutex or Suboxone, and you can go to a pharmacy and refill your prescriptions for these drugs as needed.
From a medical perspective, using buprenorphine in substitution therapy for opioid maintenance presents significant problems when a patient attempts to detox. Comparatively, ibogaine addiction interruption therapy and treatment for opioid dependence is effective for people dealing with addictions to Subutex and Suboxone. In fact, it can sometimes take 4-6 weeks or more of gradually tapering your use of buprenorphine and switching over to short-acting opioids (SAO’s), prior to receiving ibogaine therapy for opiate dependence to treat an addiction to Subutex or Suboxone.
Subutex is essentially a brand name for buprenorphine. Conversely, Suboxone presents its own unique complications relative to ibogaine treatment for detox from opiates and opioids, due to the fact that it contains the opioid antagonist naloxone. Since naloxone occupies opiate receptors within the body and displaces other molecules, it is paramount not to have any naloxone present in the body prior to receiving ibogaine therapy.
When a patient is unable to switch to short-acting opioids prior to arriving at Clear Sky Recovery’s ibogaine treatment clinic in Cancún, Mexico, successfully detoxing from buprenorphine can take between 10 days to over 2 weeks. Prior to receiving ibogaine detox therapy, we switch a patient to short-acting opiates, stabilize him or her on SAO’s, and administer multiple doses of ibogaine as required, with several days of downtime between booster doses. Please note: Clear Sky Recovery will not treat patients who are on more than 8 mg of buprenorphine when they arrive at our treatment facility.
Believe it or not, there are many ibogaine treatment clinics that make promises and are happy to take your money for an ibogaine detox that cannot possibly work when applied to a heavy buprenorphine addiction. But let’s be clear: ibogaine cannot help you detox from high doses of buprenorphine in short periods of time. Anybody who claims otherwise is significantly misrepresenting how ibogaine interacts with buprenorphine and knowingly selling you a treatment that will not have a positive outcome.
Suboxone and Subutex addiction is not an easy condition to treat. Therefore, it is important that you, your clinician, and our M.D.’s, remain in contact in the days leading up to your ibogaine treatment. At Clear Sky Recovery, we have had tremendous success utilizing ibogaine addiction interruption therapy to mitigate upwards of 95% of withdrawal symptoms related to detoxing off of buprenorphine. It is the most advanced protocol we have developed, and as such, it takes the greatest amount of time to successfully complete. To learn more about our comprehensive ibogaine therapy options, please call us today at 305.901.5371.
Put an End to Your Subutex Cravings
What to Expect from Ibogaine Treatment for Buprenorphine Addiction
In a less-than-ideal situation — in other words: the real world — when a patient is unable to make the switch to short-acting opioids prior to arriving at Clear Sky Recovery’s ibogaine treatment clinic in Cancún, successfully detoxing from buprenorphine can take between 10 days to over 2 weeks of time. Prior to receiving ibogaine detox therapy, we need to switch you to short-acting opiates, stabilize on SAO’s, and then administer multiple doses of ibogaine as required, with several days downtime between booster doses.
Please note: we will not treat patients who are on more than 8mg. of buprenorphine at time of arrival. Unless you plan to stay in Cancun for 2-3 months, it’s not going to work. Period. There are many ibogaine treatment clinics who will make assurances and promises and are happy to take your money for an ibogaine detox which cannot possibly work when applied to a heavy buprenorphine addiction, with the expectation being that you’re going to be reset in a week.
Ibogaine cannot detox you from high doses of buprenorphine in short periods of time. Anybody who claims this is possible, is at best ignorant, at worst, significantly misrepresenting how ibogaine interacts with buprenorphine, and knowingly selling you a treatment that will not have a positive outcome.
Suboxone and Subutex addiction is not an easy condition to treat, and it’s extremely important that you, your clinician, and our M.D.’s, remain in contact during the period of time leading up to your ibogaine treatment.
We have had tremendous success utilizing ibogaine addiction interruption therapy to mitigate upwards of 95% of withdrawal symptoms related to detoxing off of buprenorphine. But this is the most complicated protocol we have developed, that takes the greatest amount of time to complete successfully.
Start Detoxing From Suboxone Today
Articles About Ibogaine for Buprenorphine, Subutex and Suboxone Addiction Treatment
Ibogaine for Buprenorphine, Subutex and Suboxone Addiction: Does it Really Work?
The national heroin addiction epidemic may be the splashier headline in the news, but if you’re reading this, you already know that the Buprenorphine, Subutex and Suboxone addiction is just as dangerous and causes just as much loss. The idea that the legality or accessibility of these drugs means they are less addictive or dangerous simply isn’t true. Buprenorphine, Subutex and Suboxone addiction is opiate addiction, just like addiction to heroin. This prompts the question: does ibogaine for Buprenorphine, Subutex and Suboxone addiction really work? This post dives into the answer and the underlying facts.
If you need the details about using ibogaine to treat Buprenorphine, Subutex and Suboxone addiction, this is the page for you. This article describes how experts are using ibogaine treatment to address drug addiction, including the latest research into neurochemistry, ibogaine, and Buprenorphine, Subutex and Suboxone addiction.
How to Pick the Perfect Buprenorphine, Subutex or Suboxone Addiction Treatment Center
As you search for a Buprenorphine, Subutex and Suboxone treatment center, you might be thinking something like this: am I really in the position to make a decision about something this important? I’m here today because I’ve made bad decisions! You’re right that choosing the perfect Buprenorphine, Subutex and Suboxone treatment center is one of the most important choices you’ll ever have to make, but don’t lose hope. With the right information on your side, you can and will make a great decision—because you know what’s at stake, and you want to live.
So, how do you choose? First, you must be sure you clarify your priorities and needs and see that you’ll receive the best psychological and medical expertise during the time you spend in treatment. You’ll also need an evidence-based approach to beat your addiction to Buprenorphine, Subutex and Suboxone, along with the right mix of amenities that will allow you to rest in security and feel comfortable. Learn how to choose that kind of Buprenorphine, Subutex and Suboxone treatment center right here.
Ibogaine – A Cure for Buprenorphine, Subutex and Suboxone Addiction?
This post is a jumping off point for a news video, an investigative piece that explored the ibogaine breakthrough as it first became mainstream news. The post also offers a discussion of the video. The news report describes ibogaine as a “cure” for Buprenorphine, Subutex and Suboxone addiction, and the post provides commentary and more facts to ground the piece contextually.
Despite the way it sounds, there is no instant “cure” for drug addiction—including ibogaine. However, as you’ll see in the report, ibogaine feels like the next best thing, especially to the longtime, hardcore users who pioneered the treatment. The brain on Buprenorphine, Subutex and Suboxone gets used to a flood of neurotransmitter chemicals, and the ibogaine molecule “resets” the brain so it can get past this painful feedback loop. This means no withdrawals despite the Buprenorphine, Subutex and Suboxone addiction, and a chance to start fresh.
Learn more about how ibogaine “cures” Buprenorphine, Subutex and Suboxone addiction from the video and this post.
When to Know to Seek Help for Buprenorphine, Subutex or Suboxone Addiction
Maybe it seems like the time to ask for help should be self-evident, but anyone who has felt the pull of Buprenorphine, Subutex and Suboxone addiction knows that this just isn’t the case. The brain will go to extraordinary lengths to keep repeating experiences and maintain higher levels of neurotransmitter chemicals it wants, and this skews the judgment of the person addicted to Buprenorphine, Subutex and Suboxone. So how do you know when enough is enough?
This piece offers a detailed list of signs of Buprenorphine, Subutex and Suboxone addiction, so you can perhaps recognize your own life in black and white. It also explains why those signs add up to needing help at all and offers a way to get that help.
Polysubstance Abuse Disorders and Ibogaine
Buprenorphine, Subutex and Suboxone addiction is complicated enough on its own, but when the user is also addicted to other drugs or alcohol, the situation is even more complex. This post discusses what polysubstance abuse looks like, and how ibogaine can be used to treat it. It also describes symptoms and signs of polysubstance addiction in detail, including for those suffering from Buprenorphine, Subutex and Suboxone addiction along with other substances.
Learn the facts about ibogaine treatment for polysubstance abuse disorders and Buprenorphine, Subutex and Suboxone addiction here in this article. Find out what you can expect from the process, and how to prepare for the journey ahead.

